For screening purposes, a woman is considered at average risk or high risk for breast cancer.
According to the American Cancer Society (ACS), a woman who
does NOT have the following is considered to be at average risk:
• A personal history of breast cancer
• A strong family history of breast cancer
• A genetic mutation known to increase risk of breast cancer (such as in a BRCA gene)
• Chest radiation therapy before the age of 30
Guidelines for women who are at average risk for breast cancer:
Ages 20 - 34
- Breast self-exam once a month, one week after onset of menstruation
- Physical exam yearly
Ages 35 - 39
- Breast self-exam once a month, one week after onset of menstruation
- Baseline mammography
- Physical exam yearly
Ages 40 - 44
- Breast self-exam once a month, one week after onset of menstruation
- Have the option to start screening with a mammogram every year
- Physical exam yearly
Ages 45 - 54
- Breast self-exam once a month, one week after onset of menstruation
- Mammography every year
- Physical exam yearly
Age 55 and older
- Breast self-exam once a month, one week after onset of menstruation; post-menopausal women - the same day each month
- To discuss with your personal physician: Switch to a mammogram every other year or continue yearly mammograms. Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
- Physical exam yearly
Standard Procedures
Aspiration
Fine needle aspiration of the breast is a simple, inexpensive diagnostic procedure which is reported to be highly accurate. Breast aspiration may be performed in the doctor’s office in a matter of minutes, with a minimal amount of discomfort to the patient. The procedure is performed using a very fine needle – one much smaller than that used to draw blood from a vein. The skin when the needle is introduced may or may not be anesthetized (frozen) with a local injection. Because the results of the aspiration are available within a short period of time, it spares the patient unnecessary anxiety. Since it is a simple office procedure which leaves no scar, it is psychologically more acceptable to women than an open biopsy. If the fine needle aspiration shows no cancer cells, but your doctor notes any suspicious or worrisome mass, further tests are indicated.
Core-needle biopsy
A core-needle biopsy is a diagnostic procedure reported to be highly accurate in identifying the presence of a malignant tumor. The larger size needle used in this procedure is able to obtain tissue samples from areas where calcifications are seen on mammography. The core needle is usually guided into position with the use of ultrasound then multiple tissue samples are removed.
Mammography
A mammogram can detect lesions in breast tissue, which might otherwise go unnoticed because they are very small or deeply buried and cannot yet be felt during palpation. This makes mammography particularly valuable as a screening tool in detecting early breast cancer.
Learn more: Breast Cancer Screening
When A Biopsy Is Needed
All suspicious lumps should be biopsied for a definite diagnosis, even when the mammography findings are described as normal. Many mammographers request a woman notify the person taking the mammogram if she is taking hormones.
Microcalcification
A common sign of breast disease found by mammography is microcalcification - very small deposits of calcium, deposited in breast tissue. The calcifications are usually of varying shapes, frequently occur in tight groups, and are found in benign (NOT CANCEROUS) and malignant (CANCEROUS) conditions. Sometimes these calcifications, seen on mammogram, occur without an associated mass.
Clusters of microcalcifications are routinely biopsied. However, when the cytology (cell examination) is benign, but the type of calcification is still of concern, it may still be necessary to surgically remove or excise the calcification for tissue or histologic examination.
Mammography is considered the "gold standard" for detection of early breast cancer. Follow-up with mammography of those patients with microcalcifications is very important. The finding of a change in the pattern, or a few new calcifications, may allow early detection of a small or "minimal" cancer. This is why it is necessary to have more frequent mammography when recommended by your doctor.
Needle Localization
Sometimes very small lumps which cannot be felt but do show up on a mammogram can be very hard to locate and biopsy. In order to locate the exact site of such a small lump, a special type of needle, with a fine hookwire inside it, is guided into the lump during mammography. When the needle reaches the exact site of the lump the small hooked wire is then extended past the needle into the lump. It is left in the lump until the patient is brought into surgery for the surgical removal of the lump. By localizing the lesion, the physician is able to remove the lump without removing a large amount of normal tissue.
Open Biopsy
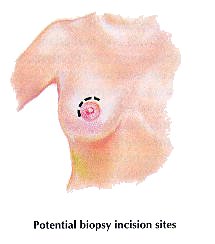
This procedure combines surgical removal with microscopic examination of the suspicious tissue. No matter how sensitive a doctor’s fingers, he/she cannot feel the difference between cancerous and non-cancerous cells; that difference appears only under a microscope. Biopsy is the most accurate method of diagnosing the nature of a breast lump, and your doctor will recommend it if he or she cannot otherwise be absolutely certain that a lump or other breast symptom (nipple discharge, dimpling, or discoloration of the skin, etc.) is harmless. It is important to remember that 80 percent of all breast biopsies do prove that the growth in question is benign.
Since most malignant lumps occur in the upper outer quadrant of the breast, this is a common site for biopsy incision. Another such site is the edge of the areola surrounding the nipple. Depending on the size of the lump, part or all of it will be removed for evaluation.
Ultrasound
Breast ultrasound is a procedure used to further evaluate a breast abnormality or lump seen on mammography. It is an imaging technique, which uses high frequency sound waves to scan the breast to locate and measure abnormal changes or lesions in the breast. Ultrasound can determine if a breast lump is solid (tumor) or filled with fluid (cyst).
Breast ultrasound is not meant to replace the mammogram. Unlike mammography, ultrasound is not able to detect small calcification.


